In the first of a new monthly series, we asked readers to help solve this case involving a patient treated for arrhythmia who develops unexplained bradycardia. Find the answers below!
Case
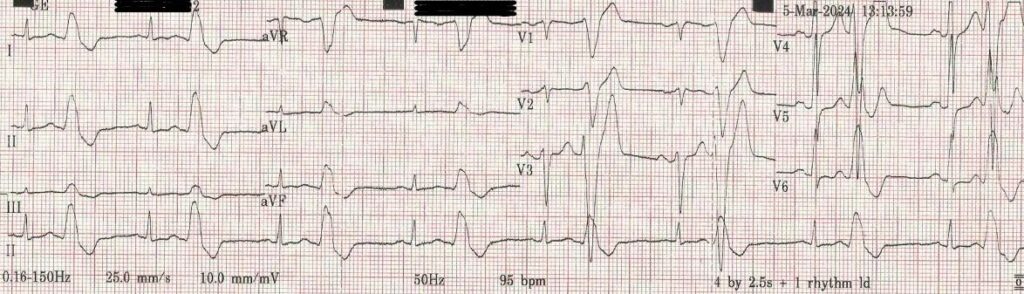
A 64 year old man is found to be experiencing multiple ventricular ectopics when a resting ECG is performed as part of a routine medical (see trace below).
He is referred to a cardiologist who arranges an echocardiogram and Holter monitor. The former reveals possible early stages of cardiomyopathy and the latter confirms a high load of ventricular ectopics comprising ventricular bigeminy, average heart rate 80-100.
The consultant asks you to start him on bisoprolol 2.5mg with the request that his pulse rate is monitored.
The patient has a BP monitor at home which provides a pulse rate and agrees to send the results in for monitoring purposes.
A couple of weeks later he provides these and you note that the pulse is consistently around 40. You contact him and are relieved to hear that he is experiencing no symptoms. You conclude that the bradycardia is a side effect of the beta blocker. As the consultant was very keen that he should be on it, you reduce the dose to 1.25 mg and repeat the process.
His further readings are identical – a pulse of around 40.
You stop the bisoprolol but to your surprise, the pulse rates he subsequently submits remain around 40 – though he still does not complain of shortness of breath, dizziness or any other symptoms. Thinking that he may have gone into heart block you arrange an urgent resting ECG. To your surprise, the result is identical to the original, with an average rate around 80.
Answer
‘Pulse rates provided by standard home BP monitors with cuffs are reliant on pulse volume to count the pulse. The volume ejected by the left ventricle in the context of an ectopic is reduced because of the lack of proper ventricular filling from the atrium. This low volume pulse may not be detected by the BP monitor. In effect, his monitor was picking up only the normal ventricular beats and not the ectopic ones – hence it gave a pulse rate spuriously half the actual value. For future monitoring he will need to use a gizmo which picks up the heart’s electrical activity rather than pulse volume, or learn to do it the traditional way.
‘Well done to the commenters, who got there a lot quicker than I did. In my defence, we’re all familiar with high noise to signal ratios in primary care and for the sake of clarity and brevity I did filter out a fair bit of the noise! But it does illustrate an important lesson in potential overreliance on, or misinterpretation of, home monitoring.’
Dr Keith Hopcroft, Pulse clinical adviser, who set the case
















