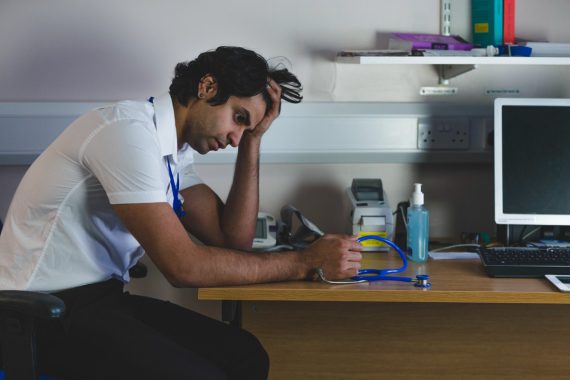
GPs continue to be the least likely to be satisfied with their job and the most likely to be struggling with their workload among all doctor groups, according to new GMC data.
The regulator’s latest annual report into workplace accounts of doctors in the UK warned that the experiences of GPs ‘remain concerningly poor’.
It found that last year, 48% of GPs ‘were struggling’ – meaning they are regularly working beyond their rostered hours and feeling unable to cope with their workload – more than any other group of doctors.
Separate GMC data shared with Pulse also showed that GPs are more likely than other doctors to be reducing their hours, with 29% reporting they have reduced their hours due to pressure on workload and capacity.
This is happening in all parts of the profession, with 19% of all doctors saying they reduced their hours and 41% declining to take on additional work.
The GMC warned that ‘years of worsening levels of satisfaction and burnout’ are leading doctors to ‘take matters into their own hands’ by reducing their hours.
‘Such moves can help safeguard patient care, for example by doctors not working additional hours if they are already exhausted,’ the GMC added.
But it warned that if the trend continues unaddressed, the capacity of already stretched health services ‘could be reduced even more, putting patients at risk’.
That GPs have worse experiences than other groups of doctors ‘has been a persistent pattern since 2019’, with only ‘small improvements’ since 2022.
The report said: ‘GPs’ experiences have been persistently worse than those of other groups of doctors. In addition, GPs with training responsibilities are under more pressure than their non-trainer colleagues.
‘Solutions must be found to address unsustainable system pressures, with specific solutions to target the poor experiences of GPs.’
It found that:
- Out of the main doctor groups, GPs were the least likely to be satisfied (42% compared with 53% of all doctors) and most likely to be struggling with their workload (48% compared with 33% of all doctors).
- Just over a fifth of doctors (22%) reported that they had to act in a way that conflicted with their personal values at least once a week. This was particularly common among GPs (31%)
- A quarter of doctors in training (24%) were at high risk of burnout.
- However, compared with previous years, GPs have seen an improvement in overall risk of burnout and, in 2023, were the group most likely to feel supported.
- Disabled doctors continue to report worse experiences than those without a disability, being more likely to be dissatisfied in their work (44% vs 38%) and consider retiring early (13% vs 7%).
- Higher proportions of doctors are reducing their hours (19% in 2023 and 18% in 2022, compared with 8% in 2021); and declining to take on additional work (41% in 2023 and 42% in 2022, compared with 23% in 2021).
- Almost a quarter of doctors (23%) took a leave of absence due to stress in the previous year, consistent with 2022 (22%), but up from 17% in 2021.
The report was based on a survey of 4,288 UK doctors, including 957 GPs.
GMC chief executive Charlie Massey said that doctors protecting their wellbeing ‘is essential’, but called for alternative solutions to reducing hours.
He said: ‘We know that when doctors are overworked and under-supported there is a risk not only to doctors themselves, but also to patient care.
‘These data show that more doctors are now taking matters into their own hands, not just to protect their own health and wellbeing, but that of their patients as well. For many, this will often be the only responsible course to deliver safe care. But this action comes with risks.
‘We must be clear that doctors protecting their wellbeing is essential, but they shouldn’t feel their only option is to reduce their working hours. This presents challenges in capacity planning, adding further pressure to services that are already stretched.’
Dr Alan Stout and Dr Andrew Buist, co-chairs of GPC UK at the BMA, said: ‘It’s unsurprising this report found that GPs are changing their working patterns. We know that many, overworked and exhausted, are being pushed to do this for the sake of their own health and wellbeing. Just this week, a BJGP study found GPs in England alone work 49.2% more hours per session than previously defined.
‘Changes to work patterns are a symptom of the pressures facing general practice. For too long, practices haven’t been given the funding they need to keep up with rising running costs, hire the staff they need, or, in some cases, stay open. On top of growing patient demand, many GPs are at breaking point.
‘Core GP contract funding must be increased, so that practices can afford to provide safe, efficient GP-led services that reduce pressure on staff. More immediately, health departments must agree a fair method for funding the latest DDRB uplift and associated overheads for all practice staff with us, or there is a significant risk of crippling practice finances even further.’
BMA representative body chair and workforce lead Dr Latifa Patel said doctors are being ‘forced to take matters into their own hands’ to protect themselves and their patients.
She said: ‘Reducing hours will be a last resort for many doctors who want to be working, looking after patients and supporting their colleagues. But ultimately, a burnt-out doctor is not a safe doctor.
’That certain groups – including disabled doctors, those from ethnic minority backgrounds, women and doctors on locally-employed contracts – are feeling the pressures worse, is an indictment of a system that is not properly supporting and protecting its staff.
‘Even with increased recruitment, it’s clear the NHS, the Government, regulators and training bodies need to do much more to support doctors and keep them in the workforce – rather than forcing them to reluctantly reduce work or letting them go prematurely.’
Medical Protection Society (MPS) medical director Dr Rob Hendry said the survey results were ‘concerning, yet sadly unsurprising’.
He said: ‘When mental wellbeing is poor and healthcare professionals cannot – for a variety of reasons – access the support they need, it can result in extended periods of time off work and some even decide to leave the profession altogether. Suffering with mental wellbeing problems can also jeopardise patient care.
‘This is why we continually called on the previous government to work with NHS England and others to ensure funding for healthcare workers’ mental wellbeing support is sufficient. Improving wellbeing is key to retention, and it is critical that we see some long-term thinking on this issue from the new Government.’
NHS providers deputy chief executive Saffron Cordery said that the report exposed ‘the enormous strain on overstretched NHS staff’.
She said: ‘Stress, anxiety and depression remain the top reasons for thousands of staff being off work sick.
‘It’s worrying that more doctors are at high risk of burnout now compared to before the pandemic and that day-to-day satisfaction among them has fallen since before Covid-19.
‘Heavy workloads, long hours, staff shortages and long waiting lists are cited while more doctors say they don’t feel valued.’
Last month, the GMC warned that plans for expanding the medical workforce ‘will fail’ if the NHS does not prioritise trainer capacity and support.
And last week, the BMA announced the results of its non-statutory ballot, which saw 98.3% of GP partners voting in favour of taking collective action from 1 August, in protest against contractual terms and funding.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens













Why would the GMC care? They have a large part in causing this. Nasty, rabidly anti-doctor cabal. Lower than vermin.
It took 18 months for my case to be thrown out. Thank you GMC for being so quick and efficient. 18 months of waiting with a tarnished reputation was just a brease! Go jump off a cliff you tossers.
Reducing hours is not helpful. Work just builds up. All gps where possible need to work full time and work load will be manageable.
A contract that caps workload is the only thing that fixes this.
We should all be able to come to work, know when we will finish and have completed everything associated with that day.
All mandatory training/CPD/QIA should also be done in this time
Another report …
The GMC is an aberrant organisation which should attract no discussion other than the focus on its abolition and enquiries into its lack of insight into its own bizarre actions.