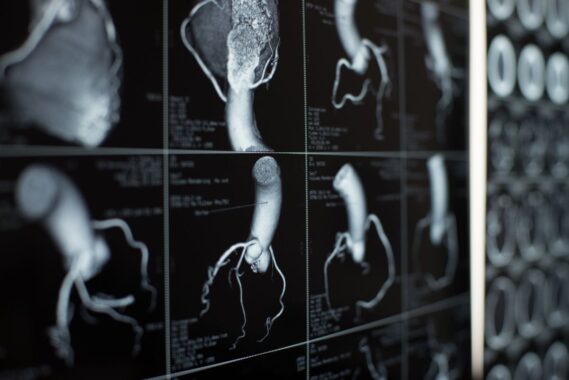
In the next of our series, GP Dr Matthew Molloy considers this hypothetical case of a man with a finding of calcified coronary arteries after lung cancer screening
You see a 62-year-old man who has recently undergone a CT scan, having been identified as high risk for lung cancer as part of the new lung cancer screening programme. The scan is negative for lung cancer but the report has flagged a finding of calcified coronary arteries with a request to follow up. He has no symptoms – in particular, no chest pain or breathlessness on exertion – and cardiovascular examination is normal.
How common is this finding in asymptomatic patients?
Lung cancer causes more deaths than any other cancer in the UK. Often there are no signs or symptoms if the cancer is at an early stage.
Patients who have ever smoked and are aged between 55 and 74 are being offered lung health checks. Currently, lung health checks are only available in some parts of England. The Government has announced that they will be available everywhere by 2029.
Lung health checks assess lung function and can help diagnose lung cancer early. Early diagnosis can make lung cancer more treatable and make treatment more successful.
Lung health check appointments may be in person, by phone, or online. Based on the results of this assessment, in which patients are questioned about health and lifestyle, they are either discharged, referred to the GP or offered a CT scan of the chest.
Commonly GPs receive reports of these CT scans, confirming that there is no evidence of lung cancer – but incidentally the scan has reported coronary or cardiac calcification. The coronary calcification may be reported as mild/moderate or severe.
How to properly manage this finding in primary care is sometimes a cause for concern and confusion.
What are the implications of calcified arteries?
Cardiovascular disease is one of the leading causes of death in the UK. Early detection of coronary artery disease can significantly reduce future coronary events and lead to a reduction in morbidity and mortality.
Coronary artery calcium (CAC) is specific for coronary artery atheroma and can be seen on CT scans of the thorax. There is strong evidence that increasing levels of CAC are associated with a worse cardiovascular prognosis and an increasing level of obstructive coronary artery disease.
A review in the journal Heart states: ‘The grading of CAC presence and severity was reproducible, and although the prevalence rose with age, prognostic and treatment implications were maintained across all age groups. CAC presence and severity detected patients at increased risk of MI, stroke and all-cause mortality and identifies a significant proportion of untreated patients. Its reporting provides a simple, opportunistic approach to risk-stratify patients who may benefit from cardiovascular risk optimisation in all age groups.’
What should the clinician do next?
The identification of coronary artery calcification indicates the presence of previously unknown coronary artery disease, and should trigger an assessment of signs or symptoms of cardiovascular disease in the patient.
In patients who have established cardiovascular disease and for those whose symptoms are properly managed and receiving appropriate secondary prevention, no further action is required. Their notes should be reviewed to ensure that they are on a high dose, high intensity statin and that their lipids are to target. If not, additional treatment with ezetimibe or new injectable treatment should be considered. Blood pressure needs to be treated to target, diabetes controlled and modifiable risk factors such as smoking, weight and exercise should be targeted.
For patients with no history of established cardiovascular disease, arrange an appointment to find out whether the patient has any cardiac sounding symptoms that the GP is unaware of. A patient with new exertional chest pain should be started (allergies and contraindications permitting) on aspirin, bisoprolol, a nitrolingual spray (GTN) and a statin and referred urgently to the local secondary care cardiology service or rapid access chest pain clinic.
The presence of coronary artery calcification warrants treatment with statins, based on consensus. Atorvastatin 40mg should be prescribed for patients with mild or moderate coronary artery calcification, for severe coronary artery calcification atorvastatin 80mg should be prescribed. In addition, undertake a further assessment. The presence of coronary calcium alone does not mean these patients are classed as needing secondary prevention.
In patients with no exertional chest pain, undertake a thorough CVD risk assessment to identify hypertension, diabetes, chronic kidney disease or any evidence of end organ damage. Blood tests should include FBC, UEs, lipids and HBA1c. Other tests include urine for ACR, blood pressure measurement, pulse check (to exclude atrial fibrillation), BMI calculation and a 12 lead ECG. Although the decision to prescribe statins has already been made, QRISK3 calculation helps ongoing management, eg in deciding whether to actively manage other risk factors, such as blood pressure, too.
The patient should then be treated and optimised and given lifestyle advice. Counsel the patient needs regarding their CVD risk, with advice and signposting to local services to help with smoking, alcohol, diet and fitness levels if needed.
Patients should be counselled about the significance of cardiac/exertional symptoms and asked to report any such symptoms as soon as possible.
Dr Matthew Molloy is a GPSI in cardiology at the Westcliffe Health Innovations primary care cardiology service in Bradford, West Yorkshire












“The presence of coronary artery calcification warrants treatment with statins, based on consensus.”
Not much of a consensus as there’s not even a consensus amongst Pulse writers. Copperfield last week said cardiology advise was that it just needed a qrisk calculation, not initiation of statin.