How low-funded practices are more likely to rely on physician associates
In the fourth part of our series on the rise of physician associates, Madeline Sherratt and Jaimie Kaffash dig deep into the data to look at the characteristics of GP practices and PCNs that are more likely to employ PAs. And the results are illuminating…
We have already reviewed the effect of physician associates on GP recruitment, the clinical responsibilities of PAs and how effective they are. Today, we are taking a look at what kind of GP organisations are more likely to take them on.
We have dug deep into the data to take a look at practice income, deprivation levels, geography, rurality and contract type. There are roughly 1,950 PAs in general practice in England – what kind of practices are most likely to employ them?
What we are looking at
The first thing to say is they some physician associates are employed directly by practices, and others – the majority – are employed by primary care networks (PCNs), usually through the additional roles reimbursement scheme.
For the purposes of this data piece, we have combined the two sets, using the assumption that PAs will be split proportionally between PCN member practices. This is not usually the case in practice, but it is the most accurate way of analysing the data.
We have also looked at two measures – the proportion of a practice/PCN’s medical workforce that are physician associates, and how many patients there are per medical staff member. Looking at both these measures allows us to differentiate between:
- practices/PCNs/areas that appoint many PAs as extra staff, but they are supplementary to the wider healthcare team (ie, where the patients per staff members are low);
- and those who are reliant on PAs provide more care (ie, where there are lots of patients per staff member).
To put it simply, the higher the bar and the point on the line graph, the worse it is for patient care.
Practice income
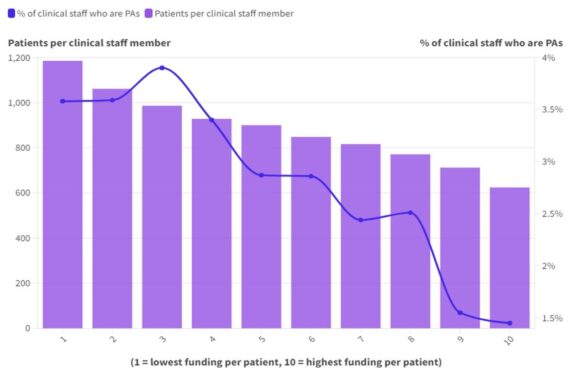
The most striking point about our analysis is how clear the link is between practice income and the likelihood of the practice and wider PCN relying more on physician associates.
We placed each practice in a decile for payments per registered patient based on NHS Digital data. Those who received the least income were in decile 1, while those who received the most were in decile 10.
The proportion of staff who were PAs in the least funded practices were more than double those in the highest funded. Not only that, but they had far more patients per staff member too.
Dr Steve Taylor, the GP representative for the Doctors Association UK, says: ‘If you have less money to go around, then some practices with simply be pragmatic about how much money they have to spend – especially when PAs are cheaper than a salaried doctor.”
Dr Farzana Hussein, GP and former clinical director for Newham Central 1 PCN, says she made the decision to the contract back for her poorly-funded practice because she refused to take the alternative option of hiring PAs. She says: ‘I ran a 5,000-patient practice Newham (a deprived area in East London) for 22 years. I left in January this year because I wanted to run a model which was still primarily salaried GPs – which I thought was safer – but I could not make the numbers work.
‘I chose personally not to have a practice-employed PA and one of the reasons for that was because I did not feel I would have enough money left over for the GP to supervise. Despite this, I feel the demonisation of PAs is wrong, and I don’t enter into that argument because doctors and PAs are brilliant in their own right.
‘The issue is that we are trying to pay for doctors and put PAs in to replace them – we’re trying to put cats into a kennel – and that is just the wrong system.’
Deprivation
There is also a link between the deprivation levels of a patient population and the use of PAs – but this wasn’t as strong as the practice income, with PAs making up roughly 3.5% of the medical staff in the more deprived areas, going down to just over 2% is the more affluent areas. There were slightly more patients per staff in the more deprived areas, but maybe not as many as might be expected.
It was noticeable that the more affluent areas were more likely to have a higher percentage of GPs than the more deprived areas. But, again, this is not much of a surprise.
Rurality
Our analysis also found that PAs are far more likely to make up a higher percentage of the medical workforce in GP practices in urban areas.
Dr Taylor says it is more likely PAs currently live in more urban areas as ‘we currently at a point in the cycle of PAs where they tend to be younger, therefore, with housing and everything else – they’re not going to be able to afford a house in the countryside.’
Traditionally, it is generally harder to recruit in rural areas, he says, but also staff turnover is more frequent in urban areas. ‘Some of it will be pay, some of it will be based on age demographics, and it may be that rural practices are more stable in terms of staff turnover because staff are more likely to remain there for a long time.’
Conclusion
It should be emphasised that, at the moment, the numbers of physician associates remain fairly low. It is unlikely that more than one in 20 medical staff are PAs even among the lowest funded practices and PCNs. But NHS England and the current Government have made it clear that this is the direction of travel, and they are looking to increase the numbers of physician associates. At the same time, there is no indication that they are going to increase funding for practices to recruit GPs – or even include GPs in the additional roles reimbursement scheme.
So what Pulse’s analysis may well show is that, as finances continue to bite, it is conceivable that more practices and PCNs will be turning to PAs to fill a gap they can’t afford to fill with GPs.
Unless the Government increases funding, it is more likely that the PA, and not the doctor, will see you now.
Tomorrow, we will be featuring a map showing how much your region relies on physician associates
Methodology
Workforce numbers
To get full workforce numbers at a PCN level, we combined NHS England’s Primary Care Network Workforce data and the General Practice Workforce practice-level data.
Practice level data
For the practice level data, we extracted the data on the total number of fulltime equivalent GPs (excluding trainees), the total number of FTE nurses and the total number of FTE direct patient care (DPC) staff, which together covers all the clinical staff. We also separately extracted data on FTE physician associates, which are incorporated within DPC staff.
We used the EPCN data to match practices to PCN as this is much more reliable than the workforce data.
Where practices were missing data on GPs and nurses, we averaged the number of patients per GP/nurse within each PCN, and applied this average to the practice accordingly.
For direct patient care and physician associates, all missing data was replaced with 0. This was because, in the majority of cases, the value was 0, so it would not make sense to use an average.
Any practices that still had no data under GPs or nurses after this was removed (ie, those with no PCN affiliation or patient numbers).
PCN level data
We removed the medical clinical director (GP), clinical director (nurse), clinical director (direct patient care) and non-clinical director figures
To get the total number of clinical staff in a PCN (and later within a practice – see below), we grouped the staff roles employed by a PCN as such:
GPs: Salaried GPs; GP Locums.
Nurses: Advanced Nurse Practitioners; Nurse Dispensers; Nurse Specialists.
Direct patient care; Other Nurses; Community Mental Health Nurses; Community Mental Health Nurses (Mental Health Practitioners); Advanced Paramedic Practitioners; Advanced Pharmacist Practitioners; Advanced Physiotherapist Practitioners; Advanced Podiatrist Practitioners; Applied Psychologists – Clinical (Non-Mental Health Practitioners); Applied Psychologists – Clinical (Mental Health Practitioners); Clinical Associates in Psychology (Non-Mental Health Practitioners); Clinical Associates in Psychology (Mental Health Practitioners); IAPT staff; Nursing Associates; Paramedics; Pharmacists; Physician Associates; Physiotherapists; Podiatrists.
We removed the following staff categories: All apprentices; All trainees; Advanced Dietician Practitioners; Advanced Occupational Therapist Practitioners (Non-Mental Health Practitioners); Advanced Occupational Therapist Practitioners (Mental Health Practitioners); Care Coordinators; Dieticians; Dispensers; General Practice Assistants; Health and Wellbeing Coaches; Health Support Workers; Healthcare Assistants; High Intensity Therapists; Mental Health and Wellbeing Practitioners; Other Direct Patient Care; Peer Support Workers; Pharmacy Technicians; Phlebotomists; Psychological Wellbeing Practitioners; Social Prescribing Link Workers; Social Workers; Therapists – Counsellors; Therapists – Occupational Therapists; Therapists – Others.
Combined practice workforce figures
We added the PCN-level figures to the practice-level figures. To do this, we worked out what percentage of a PCN’s population each practice had. We then applied this proportion to PCN-employed GPs, nurses and DPC to assign total staff numbers to every practice (ie, if a practice comprised one-fifth of a PCN’s population, and there were 10 direct patient care staff, two DPC would be assigned to that practice).
This gave us Total Practice Staff (TPS).
We also did this separately for physician associates.
Please note: we understand this isn’t precisely how PCN staff would be assigned, and recognise this as a weakness, but still felt it was the best option.
Deprivation
We used Patients Registered at a GP Practice, April 2024 – NHS England Digital and cross referenced the Index of Multi Deprivation.
We assigned the total practice staff, as calculated above, and the sub groups of GPs, nurses, DPC staff and physician associates to each mini LSOA population.
We then calculated how many patients and GPs/nurses/DPC/PAs were practising in each deprivation index decile.
Payments
We used the NHS Payments to General Practice dataset.
Removed the following practices from the dataset:
- Any that had a close date
- Any with atypical characteristics
We removed the following funding pots, as they are reimbursements, and not indicative of payments per patient.
- Premises
- Locum allowances
- Reimbursement of drugs
- All PCN funding, as this is unreliable, and could distort the figures.
We removed every practice receiving less than £50 per patient and all practices with incomplete data.
Put remaining practices in payment deciles based on how much funding they received per registered patient.
Please note: we understand that it would be helpful to understand how much each practice received through PCN funding before assigning them to deciles, but there is no accurate way to do so.
We used this same dataset to assign rurality type to each practice.
Map
For our map, which will be published tomorrow, we decided to use CCG area, as this was bigger than PCN level, but also small enough to provide meaningful data. We felt ICB level was too big.
To match practices (and TPC) to CCGs, we used the EPMC dataset.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [2]
Please note, only GPs are permitted to add comments to articles














Good job but even though, as per your caveats, the methodology, sampling, data collection etc is open to critique, the clear take home point is that poorly funded practices are more likely to accept the “gift horse” of ARRS.
Hopefully GP practices WILL look the gift horse in the mouth and see it for the Trojan horse it is, sent in to destroy traditional general practice, and GPs will look to the longterm and refuse to take on ARRS, but ask for the funding to appoint trained nurses and GPs instead. Those practices that take on ARRS roles, which haven’t even been subjected to due diligence in their establishment, are only helping NHSE destroy their own profession…
Not having a go at ARRS who have unfairly been used as pawns by Govt.
Physician associates (PAs) are increasingly being used in GP practices, especially those with lower funding. The data shows that less funded practices and those in urban areas are more likely to employ PAs due to their lower cost compared to salaried GPs. This trend is worrying because it suggests that financial constraints, not patient care, are driving staffing decisions. While PAs can be valuable assistants to GPs, they cannot replace the expertise and comprehensive care provided by fully trained GPs. To ensure high-quality patient care, the government should increase funding for practices to recruit and retain more GPs instead of relying heavily on non-medics.