Analysis: SAS to the rescue?

The GMC has proposed a radical solution to the GP recruitment crisis – removing restrictions on secondary care doctors working in primary care. Jaimie Kaffash looks at the implications
For the sake of the UK, we can only hope new chancellor Jeremy Hunt has improved his head for numbers since 2015, when he said he wanted to increase the GP workforce by 5,000 in England. For those keeping count, we are currently 1,850 full-time equivalent GPs below the September 2015 figure.
No workforce initiative has really worked. We’ve had £20,000 golden hellos, incentives for GP retainers, an international recruitment drive and attempts to make it easier for leavers to rejoin the profession among others.
Now, the GMC has dared to come up with a radical UK-wide solution, and GPs can only hope that this last throw of the dice will win. It is recommending a change in legislation to allow secondary care staff and associate specialist (SAS) doctors to work in general practice.
The BMA GP Committee has said this will ‘rightly trigger a debate’ on SAS doctors working more closely with GPs.
Yet it’s not without its controversy, with fears around a lowering of standards and many warning it could lead to a return to the time before GP training became mandatory.
‘Ten thousand or more new doctors’
But for the GMC, the rationale is clear: there are already 64,000 SAS doctors working in secondary care and they have grown by 40% in the past five years – at the same rate, there will be 50,000 more in five years’ time. The GMC estimates they will be the largest cohort of doctors in the NHS by 2030. These are doctors who are skilled but are below consultant level and not receiving training. It is a diverse cohort, but they are predominantly internationally trained doctors whose qualifications don’t apply in the UK.
Such a move has the potential to revolutionise general practice. Whereas the focus has been on recruiting other healthcare professionals to ease the burden on GPs, these doctors will be more qualified than the likes of healthcare assistants and physician associates. Furthermore, it would take only a fraction of the SAS workforce to move in order to significantly bolster numbers within general practice.
If the move happens, it would be up to the SAS doctors themselves to leave secondary care and join general practice. On this, the GMC is optimistic. There is currently a high rate of SAS doctors leaving the UK – 53% of SAS doctors in 2013 were no longer practising in the NHS in 2021. The GMC says this is in large part due to fixed term contracts for many of the secondary care roles they take – which won’t be a factor in general practice.
‘We’ve essentially got a bit of the care system that we know is desperately in need of workforce in general practice, and we’ve got a massively increasing number of doctors who are prevented by red tape from being able to work there. So, let’s remove that red tape, and then work out who and how many and in what way and how quickly we’re able to move people into primary care,’ Charlie Massey, chief executive of the GMC, tells Pulse.
How many more doctors could this provide to general practice? ‘We’re into the thousands, certainly. And, I think it’s possibly even into the ten thousand or more over [the next seven to eight years], that would make a real difference to GPs and primary care.’
These plans are still in their infancy. Currently, it is just a recommendation from the GMC. It will have to be ratified by the UK Government in England, and the devolved nations parliaments through secondary legislation – although this will be a relatively short process, if there is support.
How an SAS doctor can fit in your practice
If the proposals go through, GP practices would need to provide adequate supervision for these staff and associate specialist doctors. But SAS doctors will be able to prescribe and monitor many patient needs, improving the option for face-to-face care, and could enable GPs to spend more time on complex patients. Practices could offer permanent positions to these doctors, giving patients continuity of care.
Fully qualified overseas doctors would be a great resource but at present there is too much red tape and the need for Tier 2 sponsorship, and few practices have a full understanding of what is involved.
Ash Higgs, managing director of MCG Healthcare Recruitment
Route back
After this, doctors will be free to go on the GMC general practice register and work in general practice. According to Mr Massey, it is most likely that these will initially be doctors with more generalist skills: ‘Think about an SAS doctor who is working in a hospital in terms of care of the elderly, or a paediatrician – it’s not hard to see how those sorts of doctors might be able to be deployed really effectively in a primary care environment.’
However, he adds, ‘others too’ might be appropriate for general practice: ‘People who work in emergency medicine, for example, who would be very deployable into primary care. Of course, every situation will be varied and it will depend a bit on the size of the practice as to what sorts of roles might be most appropriate for those doctors to fulfil.’
It may even enable GP practices to recruit directly from abroad, without the worry around transferable qualifications. Mr Massey says: ‘It could be that those roles would be sourced from doctors already working in the UK, in existing SAS roles. But it could open the door to doctors landing in those roles from overseas as well.’ However, he adds, this will be another issue up for discussion.
For some GPs, this could provide a significant boost. Dr Abdul Hafeez, a GP in Wrexham and founder and chief executive for the Association of Pakistani Physicians and Surgeons of the UK, says he had spoken to his health board about recruiting SAS doctors for his practice, but the current rules don’t allow it. ‘SAS Grade is a well-recognised post in hospital settings and these doctors work under the supervision of a consultant and are an important part of NHS workforce,’ he says. ‘They would be able to treat even those patients who allied health professionals cannot.’
Dr Hafeez points out another potential benefit – it will provide a route for the thousands of former GP trainees who failed at the clinical skills assessment or recorded consultations assessment parts of the MRCGP exam. These have disproportionately been international medical graduates and non-white UK GPs.
‘After discharge from training these doctors have to go back and start training in another speciality from scratch, providing they can secure a training post,’ says Dr Hafeez. ‘Some opt for just locums in A&E or other specialities but their heart is still in general practice.’
Mr Massey agrees that it could provide a route back, adding that general practice is ‘incredibly high stakes, because if you don’t get your MRCGP, the door is then firmly shut in terms of an ability to work to your level of clinical ability in a primary care setting’.
At a glance: GMC chief executive Charlie Massey on…
Solving the GP recruitment crisis…
We have this enormous supply or enormously increasing supply of SAS doctors, yet none are able to work in primary care because the performance list constrains that just to GPs.
The potential increase in the GP workforce…
We’re into the thousands… possibly even into ten thousand or more.
The type of SAS doctors who could help…
It’s not hard to see how an SAS geriatrician or a paediatrician might be able to be deployed really effectively in a primary care environment.
Supervision of SAS doctors in primary care…
Many, if not all, would be working under the supervision of GPs. But I think that’s exactly the sort of issue that we need to thrash out.
Failed GP trainees…
It’s incredibly high stakes, because if you don’t get your MRCGP, the door is then firmly shut in terms of an ability to work to your level of clinical ability in a primary care setting.
The effect on secondary care…
Over the next seven or eight years, we expect there to be about 50,000 more SAS doctors joining the NHS. So, surely we can deploy a proportion of that into primary care without adversely affecting secondary care?
Integration…
The boundaries between primary, community, secondary care will become greyer. Yes, the rules, at the moment, maintain very rigid boundaries in terms of who can work where.
Recruiting from overseas…
It could be that those roles would be sourced from doctors already working in the UK, in existing SAS roles, but it could open the door to doctors landing in those roles from overseas.
Lowering of standards?
Yet this also highlights the problems with the proposals: that a reliance on non-fully trained doctors might lead to a lowering of standards.
‘SAS doctors are quite incredible in their capabilities and flexibility,’ says Dr Dean Eggitt, chief executive of Doncaster LMC and a former GPC negotiator. ‘I am sure that they would make very able colleagues in primary care and would be very welcome to join the workforce – Lord knows we need them. But they aren’t GPs.’
In effect, this is ‘going back to the situation before GP training was mandatory’, says Professor Azeem Majeed, professor of general practice at Imperial College.
This means that it is unlikely that these doctors will be unable to work autonomously. ‘It’s a policy that will need careful evaluation,’ says Professor Majeed. ‘The doctors in these roles will also need a lot of support, supervision and professional development.’
This is something Mr Massey acknowledges: ‘SAS doctors are not the same as GPs.’ He adds: ‘The vast bulk of SAS doctors, as I understand, do work under the supervision of consultants… so many, if not all, would be working under the supervision of GPs. But I think that’s exactly the sort of issue that we need to thrash out.’
This suggests that the impact of such roles will be closer to the recruitment of other healthcare professionals – who are being recruited under the additional roles reimbursement scheme (ARRS) in England – than extra GPs. And closer still to GP trainees, who are supernumerary, with the downside that these SAS doctors won’t become completely autonomous GPs after three years. Therefore, it may not be the lowering of standards that is the problem – rather that this measure to reduce GP workload will require a lot of work itself.
Professor Martin Marshall, chair of the RCGP, says: ‘Ultimately, expansion of the wider practice team must not be seen in isolation as a solution to the chronic shortage of GPs, especially when it is GPs who supervise their work.’
With SAS doctors coming in, there is a concern that these will be GPs ‘on the cheap’. Dr Ujjwala Mohite, chair of the BMA UK SAS committee, says that SAS doctors are currently not valued highly enough. However, she adds: ‘Such a plan should not be a case of employing largely international medical graduates cheaply and on poor terms to plug staffing gaps, as we see with many locally employed doctors.’
There are other ethical considerations, too. First, there is the possible effect on secondary care, which itself relies on these doctors. Mr Massey is fairly sanguine on this: ‘Over the next seven or eight years, we expect there to be about 50,000 more SAS doctors joining the NHS. So we can deploy a proportion of that into primary care without adversely affecting secondary care.’
However, on the issue of a brain drain from other countries, he is a bit more circumspect. ‘Our job at the GMC is not to get involved in recruitment, our job is to provide a seamless process,’ he says. ‘It is an important issue, but it’s probably not for us to answer.’
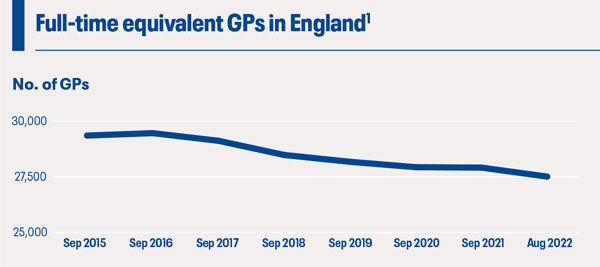

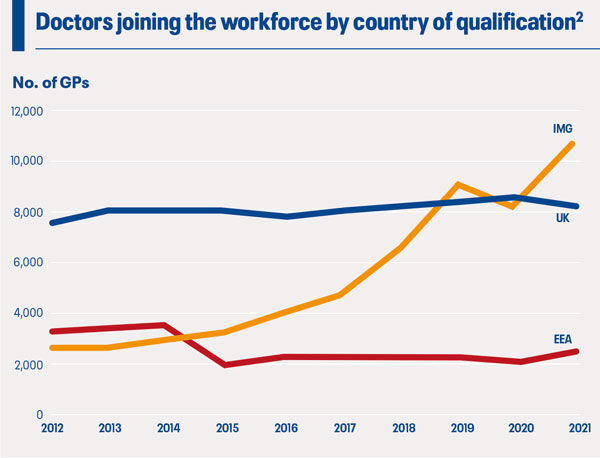
Sources: 1. NHS Digital, General Practice Workforce, 31 August 2022; 2. GMC, The state of medical education and practice in the UK: The workforce report, October 2022
Different form of general practice?
There is another potential way this could play out. It may actually be the next major step towards primary, secondary and community care coming together.
The review earlier this year into next steps for general practice by Dr Clare Fuller, a GP and chief executive of Surrey Heartlands Integrated Care System, recommended that urgent same-day appointments could be dealt with by ‘single, urgent care teams’. This could be a potential area of deployment for SAS doctors that would utilise their talents.
But Mr Massey goes further: ‘I think the boundaries between primary, community, secondary care will become greyer. The rules at the moment maintain very rigid boundaries in terms of who can work where. So we need the rules to change to enable us all to reach sensible conclusions about how can we create the right mix of workforce that’s going to support primary care.’
There are details in this proposal to be ‘thrashed out’. But if these go through, they may be the first step towards a very different general practice – for better or for worse.
Pulse July survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [8]
Please note, only GPs are permitted to add comments to articles













If the bucket is almost empty, you can certainly look at trying to top it up as best you can. And/or, you could look at why there are so many holes in the bottom of the bucket.
No, second thoughts that’s too obvious really. And too hard of course. You’d need to unwind the damage done by CQC, A&R, pensions, complaints, media vilification, political interference, NHSE, misguided targets, GMC mishandling, etc, etc…
Much better to reach for a sticking plaster.
SAS doctor is a cohort of mostly IMGs who are forced to work without progression by the NHS and Home Office . they do not leave because of a FIXED term Contact. In fact, inherent bias i the NHS recruitment and progression is the problem. In 2008 non british doctors were not allowed to train…
I don’t think this will lead to an improvement in ‘satisfaction’ amongst the uninformed public with general practice. People ‘expect’ stuff from a GP they won’t be getting from Drs who have little training in General Practice. No doubt there will all sorts of ‘explanations’ after the event from undertrained Drs about why they get so many complaints and GMC investigations. The depressing likelihood is that ‘absence of appropriate training’ will be toward the bottom of the list of reasons given for their failure
what about increasing the pre-registration period for new graduates to 3 years, with 2 of them to be spent in general practice, amd any not getting a good report from theor GP supervisor to be unable to progress into surgical specialty training?
They would have more up to date general knowledge and GP experience as students, than would overseas-train specialist doctors; and possibly more interest in learning the necessities than someone who has come to Britain specifically to gain experience in one particular kind of endoscopic nasal surgery or PET-guided ablation therapy!
For heavens sake just talk to the early retirees and leavers. It’s a simple question: “What would make you stay?” Have we ever (ever!) done a single exit interview on a single GP to try and understand the problem? I doubt it.
Pathetic and disgraceful from the regulator once more.
Perhaps a more useful plan by the GMC to develop conversion training and assessments to ensure that the SAS doctors are suitably equipped.
Instead leave them and supervising colleagues exposed to risk.
Yet again acting in the interest of the government rather than patients.
Perhaps if they had been more positively engaged prior to this crisis we would not be facing collapse of primary care services in as many areas?
You’d need to unwind the damage done by CQC, A&R, pensions, complaints, media vilification, political interference, NHSE, misguided targets, GMC mishandling, etc, etc…..all government stoogery………and nothing to do with improving patient care.
Why not just encourage current fully qualified GPs to stay ?
How?
Well here’s 3 simple ideas:
1) Get rid of appraisal and revalidation
2) Give extra funding to general practice without all the box ticking and strings attached
3)Stop CQC inspections being routine.
Enact the above and the flow of GPs retiring will slow for certain