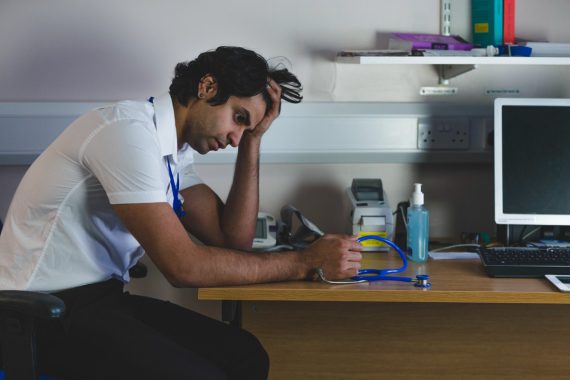
More than three quarters of GPs say they have continued to work despite not feeling well enough due to mental health concerns, a new survey has revealed.
GPs cited reasons such as staff shortages, the guilt of putting pressure on other colleagues, or because ‘it is just what is expected of them’, according to the survey conducted by the Medical Protection Society (MPS).
The protection organisation surveyed 1,075 doctors in the UK – including 255 GPs – on presenteeism in the medical workforce.
It found that 76% of GPs said they ‘have gone to work’ or ‘continued to work’ despite ‘not feeling mentally well enough to do so’.
And 68% said that this led to a lack of empathy with patients, while almost half (48%) suspected it may have contributed to a lower standard of care.
One GP taking part in the survey said: ‘Given that the system is facing near collapse, there is an unwritten sense of obligation to put in both extra hours and come to work when you might not be feeling well.
‘If this was any other industry, I would not feel guilty taking time off, but as we are dealing with some of the most important moments in people’s lives and knowing that might not be anybody else to help them, it does tend to push you into work. Essentially what I’m saying is, the NHS runs on goodwill and guilt at the moment.’
MPS said it is ‘particularly disappointing’ that over a quarter (27%) of GPs feel that taking time off for mental wellbeing issues is not ‘acceptable’ where they work.
The medical defence organisation stressed that the upcoming abolition of NHS England ‘must not hold up’ current plans to ensure mental health support services across the NHS are ‘properly funded’.
The survey findings
- 76% of GPs in the UK say they have continued to work despite not feeling mentally well enough to do so.
- 70% say they have continued to work when not feeling mentally well enough because they feel guilty adding to colleagues’ workloads;
- 51% cite staff shortages;
- 47% say it is what is expected;
- 46% say it is because their patients rely on them.
- 68% said this has led to a loss of concentration (57%) or practising defensive medicine (57%).
- 15% said it may have resulted in a missed or incorrect diagnosis.
- 18% said there had been no effect on patients.
Source: Medical Protection Society
Another GP told MPS that if they have time off due to mental health issues such as anxiety, depression, or burnout ‘people will imply that you “lack resilience”’.
And one comment from a GP received as part of the survey said: ‘I have to keep working, my partner colleagues need me to, my receptionists need me to, my nurses need me to. The practice cannot run otherwise.
‘There is always a need to provide more and more appointments, to constantly provide access. It’s endless. I cannot let my colleagues down or alone to deal with the daily aggression from patients.’
MPS president Professor Jane Dacre said that GPs are ‘notoriously reluctant to take time off when they feel unwell’ but it is ‘concerning’ that ‘so many’ continue to work despite mental health concerns.
‘If they do not feel they can take time off to recuperate or seek support – due to staff shortages or cultural expectation – this could exacerbate the issue, result in them taking more time off in the long term, or even leaving the profession,’ she warned.
On the abolition of NHS England, Professor Dacre said: ‘One year ago, NHS England initiated a review into the provision of mental wellbeing support for staff across the NHS.
‘The abolition of NHS England and the restructuring of how the NHS is managed, must not hold up a plan being implemented that ensures support services are properly funded and safeguarded.’
In response to the survey findings, the RCGP said that burnout is a ‘huge issue’ in general practice and a ‘major barrier to retaining hard-working and experienced GPs’.
Vice chair Dr Victoria Tzortziou-Brown said: ‘It’s worrying to hear that so many GPs are working when they aren’t well enough to do so, but it isn’t surprising as we know that GPs want the best for their patients, and don’t want to let them down.
‘Nevertheless, it shouldn’t be necessary and it is a symptom of an overstretched workforce dealing with unmanageable workloads.’
She said that the upcoming 10-year plan for health needs to bring ‘serious investment in general practice’ including retention initiatives for GPs.
Last year, NHS England extended the contract for a national mental health support service available to GPs – NHS Practitioner Health – after a controversial proposal to cut funding.
In 2023, Pulse reported that around one in 20 GPs in England were accessing NHS Practitioner Health services.
Pulse October survey
Take our April 2025 survey to potentially win £200 worth of tokens












I read this as three quarters of GPs don’t feel mentally well enough to work?
Is this not against GMC guidelines which says you shouldn’t work if your health compromises patient safety.
Hmmmm – not sure the GMC comment particularly helpful – this kind of comment is why people stay silent ( until often they can’t take it any more )