GP cardiology specialist Professor Ahmet Fuat outlines principles and best practice in diagnosing and managing hyperlipidaemia in primary care
Learning objectives:
- Understand the key tests and investigations required in patients with elevated blood lipid levels.
- Improve awareness of the appropriate care of patients reporting side effects with statins, and strategies to manage statin intolerance.
- Understand current expert consensus on supporting patients with hyperlipidaemia to achieve target reductions in lipid levels for both primary and secondary prevention.
- Recognise the limitations of, and how to interpret, QRISK3 scores in guiding treatment decisions.
- Gain confidence in management of specific cohorts including the very elderly and those with suspected familial hypercholesterolaemia.
1. Should all patients with apparent hyperlipidaemia have further blood tests to rule out an underlying cause such as diabetes or hypothyroidism?
Yes, it is generally recommended that patients with apparent hyperlipidaemia undergo further blood tests, to rule out underlying causes. Hyperlipidaemia, characterized by elevated levels of lipids in the blood, can often be secondary to other conditions.
Two common underlying causes are diabetes and hypothyroidism:
- Diabetes Mellitus
Insulin resistance and hyperglycaemia in diabetes can lead to dyslipidaemia, typically characterised by elevated triglycerides and low HDL cholesterol.
- Hypothyroidism
Hypothyroidism can lead to hyperlipidaemia by reducing the body’s ability to metabolise lipids, resulting in increased levels of LDL cholesterol and triglycerides.
A practical approach to testing includes the following steps.
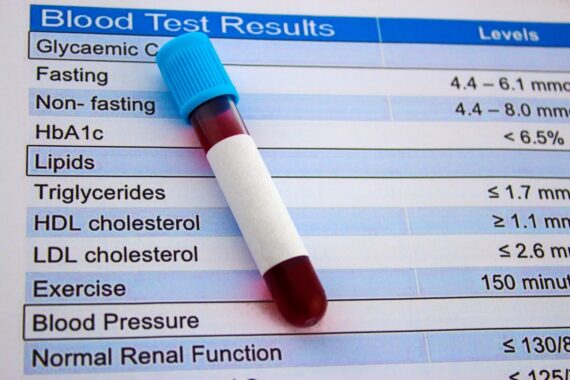
1. Initial lipid panel:
- Total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides.
2. Additional tests if hyperlipidaemia is detected:
- HbA1c to screen for diabetes.
- TSH and free T4 levels to assess for hypothyroidism.
- Renal function and eGFR.
- Transaminase level (ALT or AST).1
Identifying and treating any underlying conditions such as diabetes or hypothyroidism can improve the overall management of hyperlipidaemia, potentially reducing the risk of cardiovascular disease (CVD) and other complications.
2. In patients who are apparently intolerant of first-line statins but are willing to try another, what is a rational approach in terms of what to try next, and at what dose?
In patients who report significant side effects with first-line statins but are willing to try another, there are several steps you can take to optimise their tolerance and effectiveness, summarised as follows:2
1. Confirm statin intolerance:
- Assess symptoms. Confirm that the adverse effects are indeed due to statins and not due to other medications or conditions.
- Consider drug interactions. Review all medications to identify possible interactions that might exacerbate statin side effects.
2. Switch to a different statin:
- Some patients may tolerate a different statin better. Consider switching from atorvastatin or simvastatin to a statin with a different metabolism pathway (see next point).
- Try hydrophilic statins, ie, rosuvastatin or pravastatin, which are less likely to cause muscle symptoms as they do not penetrate muscle cells as readily as lipophilic statins like simvastatin and atorvastatin.
3. Alternative dosing regimens:
- Dosage adjustments: start with the lowest possible dose and gradually increase it as tolerated.
- Some patients tolerate alternate-day dosing better than daily dosing.
- Intermittent dosing. For very sensitive patients, try dosing every third day or even once a week, depending on tolerance and lipid level response.
4. Monitoring and follow-up:
- Monitor symptoms and lipid levels at least annually or 2-3 months after initiation or medication change: check the patient’s lipid profile and monitor for any adverse effects. NICE guidelines suggest a 40% reduction in non-HDL cholesterol from baseline in primary prevention, and targets of <2.1 mmol/L LDL cholesterol or <2.7 mmol/L non-HDL cholesterol for secondary prevention.3
- Patient education: Educate the patient on recognising side effects and the importance of adherence to therapy for CV risk reduction.
By tailoring the statin therapy approach, many patients can achieve lipid-lowering goals with minimal adverse effects. Always involve the patient in the decision-making process and ensure they understand the importance of managing their cholesterol levels for long-term CV health.
Click here to read and complete the full CPD module and download your certificate logging 2 CPD hours towards revalidation
Professor Ahmet Fuat is a GPSI in Cardiology in Darlington, Honorary Professor of Primary Care Cardiology at Durham University and education lead at the Primary Care Cardiovascular Society