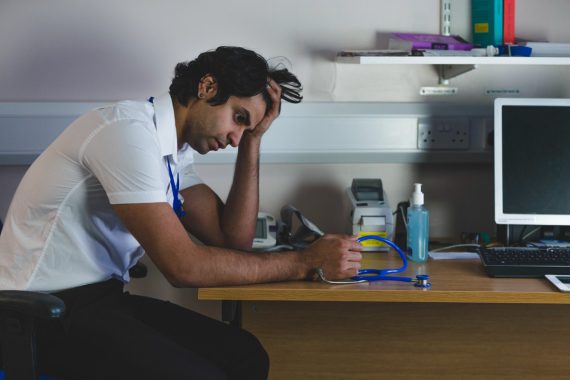
The pressures of the pandemic led to signs of psychological stress and burnout among GPs, say researchers who did a series of interviews with those at different stages in their career.
Work-related stress and anxiety were widely apparent during in-depth interviews with 40 NHS GPs including low motivation, feeling overwhelmed, frustration and anger.
Several described a ‘feeling of dread going into work’, the research published in BMJ Open found.
GPs feelings changed over time as many were focused on adapting to new systems but also uncertainty about what was ahead in the early days of the pandemic.
But as time went on the anxiety related to unmet patient need, delayed presentations and growing demand, particularly for mental health support, researchers reported.
At the same time, negative patient perceptions and media portrayal of practices being ‘closed’ increased GPs’ work stress and reduced job satisfaction, the interviews revealed.
Many GPs also described the negative impact on their families and relationships and said they were worried about the quality of patient care they provided at times of extreme fatigue.
While the interviews were done in 2021, the researchers at the University of York pointed out that since that time, further tensions in general practice have arisen, particularly regarding negative and misleading media portrayal.
Some GPs – mainly women, the researchers noted – had reduced their clinical sessions or developed portfolio careers as a way to manage the pressures and support their own wellbeing.
Women may benefit from targeted interventions to support their wellbeing and encourage continued participation, the researchers said.
And GP partners may also require targeted support as they described greater pressures associated with management workload, staff shortages and vaccination rollout.
Concerns were also raised by GP trainees on feeling of isolation and disruption to their training.
There were some positive findings with some explaining the pandemic and the vaccine roll out was an opportunity to step up and created a sense of camaraderie.
But overall, the detrimental impact of the pandemic on GP wellbeing has wider implications for workforce retention and patient safety, the researchers concluded.
It comes as worrying new data showed more than one in five GPs under the age of 30 quit the profession last year.
Looking at the ABC of doctors needs – autonomy, belonging and competence – all three have been affected by the pandemic they added.
‘GPs’ ability to control and influence their work has reduced, and patient frustrations and media blaming of GPs has affected their sense of belonging and competence.
‘There is a need for policy to support GPs, prevent work stress and foster collaborations across wider teams,’ they said.
Study leader, Dr Laura Jefferson, a research fellow at the University of York, said: ‘GPs were experiencing problems with excessive workloads that were affecting their wellbeing before the pandemic.
‘Our study explored GP wellbeing during the first year of the pandemic, highlighting how this evolved over time as GPs faced different challenges.
‘Further tensions in general practice have since arisen, particularly regarding negative and misleading media portrayal, and substantial challenges to GPs remain.’