An ICB has drawn up plans to overhaul acute care in its area, including mandatory appointment booking for A&E departments and triage though ‘neighbourhood hubs’.
Cambridgeshire and Peterborough ICB said it is planning to launch pilots of the strategy from December, aiming to shift from ‘traditional acute care to a community-based approach’.
According to a draft of the strategy, seen by Pulse, other than for blue light emergencies, patients will not access any A&E department ‘without a booked appointment slot’.
It also suggests:
- Acute triage being delivered through ‘neighbourhood health hubs’;
- An extra emphasis on patient self-care, which will involve advice from the health hubs;
- Using AI to help triage patients to primary and secondary care services;
- Bringing in locally negotiated GP contracts;
- Topping up funding for GP practices that lose out from the Carr-Hill formula.
This follows similar plans in other ICBs, aimed at bringing in reforms to acute care suggested by NHS England clinical director Dr Claire Fuller.
It is unclear from the Cambridgeshire and Peterborough plans whether acute care will be removed entirely from GP practices.
For emergencies, patients will still be able to call 111 or an ambulance and they will be given assessment by ‘a trained person’ who will be a ‘single point of access’ for them while they are ill.
It added: ‘In order to ensure we are using all channels for treating people, we need to review access to emergency departments – the first step to this is for all people not arriving by blue light to have an appointment. People will not access any ED department without a booked appointment slot.
This means the MDT and case managers can book people into the department. People as walk-ins will be assessed by the equivalent of the MDT at the front door, with the senior clinical team and be booked into the appropriate service and given the details of people who will be available to support them if there is a problem with the onward treatment point.
‘This is different from the current pathway because people are now triaged and told to wait as long as it takes.’
For non-emergency care, the document provided a series of pathways that involved patients completing ‘a short form’ on the website to ‘receive personalised information’ to help them ‘understand their condition’, or to ‘check for red flag symptoms’.
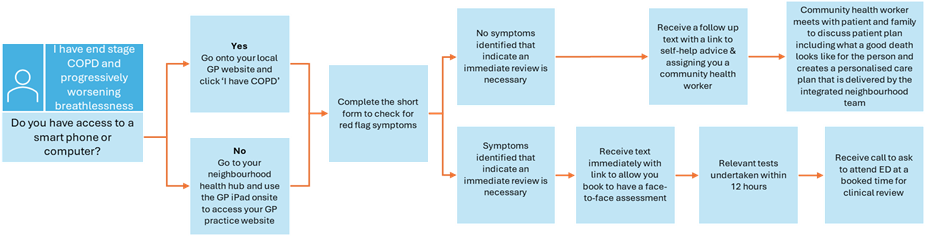
GPs will have ‘an integrated neighbourhood team’ that will ‘provide intensive support’ for the ‘most complex’ patients and ‘pro-actively’ manage their care.
They will have ‘additional capacity available outside of the practice’ to do tasks ‘not needing’ to be done in the surgery, without ‘negative financial impact on practice sustainability’.
The ICB acknowledged that the Carr-Hill formula is ‘not providing an equal playing field’ for practices and said it would use the investment fund created by the model ‘to level up payments for practices based on health inequalities and deprivation’.
The document said: ‘Of the 87 practices, the 3rd most deprived is the 66th worst funded, in the top 20 shown, 60% are in the bottom half of per patient funding.
‘This programme would address this and level up to ensure practices sustainability whilst giving patients increased access to their GP or an alternative provider for their needs.’
The plan also said that GPs are ‘fundamental’ but ‘hold a level of personal financial liability that other clinicians don’t’.
‘To ensure we can progress this model it is therefore critical that we underwrite the risk for GP practices and enable them to change,’ it added.
‘Firstly, we would propose that locally at an ICB level we have the flexibility to introduce local contracts that would be supported by our practices and our LMC. These contracts would give parity to other providers in providing financial stability over a five year period.’
Pulse has contacted the ICB for comment.
Pulse has also asked the ICB to clarify if under the plans patients would still be able to contact their practice as normal but the ICB has yet to respond.
Earlier this year, Pulse revealed that an ICB is working on plans to overhaul its GP model, which would see patients triaged by 111 call handlers and seen in a ‘neighbourhood hub’.
It comes after North West London ICB was forced to shelve similar plans for same-day access hubs, aimed to ‘deliver a single point of triage for same-day, low complexity’ demand for all 2.1 million residents within the integrated care system, leaving GP practices with only longer-term, ‘complex’ care.
It is however still planning to overhaul its primary care model by April 2025 and it has indicated it will not consult on plans as same-day hubs are a ‘national imperative’.
Pulse has reported on other areas implementing similar models, including in Cornwall where retired GPs will staff hubs to ease on-the-day demand, and Oxfordshire where ‘non-complex’ patients will be dealt with at same-day hubs.















Will they be looking for GPs to read appropriate sections of the surgical text-book over the phone to patients doing their own self-care surgical operations under alcohol ?
Seems a great idea. Triage is a bit is tricky . You can never asses all patients by triage only. They should be seen if patients desire. Patients are not capable of assessing their own conditions. Good to see this plan. Certainly improvement on what we have now ,which is dismal. Hope not long queues on phone to get tribe.
I’d be really interested to know the educational and training background of the individuals responsible for coming up with these flow charts.
Chair of CPICB has extensive history with KPMG. NHSE has been vying to exclude A+E walk-ins.
The future is giant callcentres with little clinical input, likely run by private sector and rubbish software. It will not involve GPs. It should be obvious to anyone with medical experience that these plans will be extremely inefficient, worsen accuracy of consulting, lead to patients getting the run-around, and will paradoxically increase ambulance call-outs.
Algorithm Medicine is not going well imo: personal local experience of 999 ambulances refused following 1) Stroke, 2) Broken neck (unstable fractures), 3) Subarachnoid Haemorrhage (died 1 week later).
We can either agree that KPMG/McKinsey model is the future or we can decide that we want real Medicine by real professionals. When AI starts to produce acceptable equivalence we’ll let you know.
Triage not tribe
Pulse can you please do a FOI request on how much management consultants were paid for this plan and which one/s?
It seems implicit in this model of “care” that GPs (possibly recently retired as in Cornwall) will volunteer to staff these hubs. NHS 111 and similar algorithms have a bad track record in differentiating the nuances of Acute care, and the fine line between Urgent care and a clinical Emergency. The clinical and medicolegal risk will rest with the GP who signs off a triage decision taken by a call handler. Perhaps PCN and ICB CDs should be required to take on these sessions “pour encourager les autres”?
Looking forward to seeing that end stage COPD patient with worsening breathlessness (and presumably finding it difficult to get from the bedroom to the toilet) jogging down to the local health hub to use the onsite GP iPad. Good luck with that.
Bit bemused by the flow chart that seems to offer two options- a good death or ED appointment at a booked time?
As we all know, patients do not fit neatly into boxes, and may exaggerate symptoms to subvert pathways. If the underlying issue is demand exceeding safe capacity, why will this not just displace the unsafe workload to a community hub? Where there is presumably not emergency equipment suitable to deal with severe and life threatening conditions? Could it be that the nhs model will permanently remain overwhelmed until patients have to contribute in some way? Pushing people around and making them fill endless online forms only risks the most vulnerable falling through the cracks and dying in undignified, avoidable circumstances.
Welcome to the NHS! Care is free, you just can’t get it!
This is so out there in cukooland, it is hard to fathom whixh idiots came up with this. Whoever did has no concept of managing healthcare and in particular has no idea about basic clinical care. Patients don’t fit into neat boxes and algorithms. People are complex beings and diagnosis is not simple, often there is multimorbidity and things will be misdiagnosed leading to abysmal failure of care.With this pathway, It does really seem like acute emergency care will be either a booked appointment the next day or you will be encouraged to die at home so where do the “real emergencies” go? Ill patients will drop like flies. Totally bonkers and cleelry a strategy to block medical care.
Must be really thick but the chosen flowchart seems rather IT based even if no IT skills/access.
Minor additional issue would be; I have severe COPD & Dementia & those with LPA are not local.
What is Plan C here please??
Show me the evidence. These people are not scientists. And if they are clinicians they should be ashamed of themselves.
This plan to make A&E appointment-based and triage through ‘neighbourhood hubs’ seems pretty impractical. It’s just going to create more bureaucracy and delay care for patients who need immediate attention. Plus, expecting people to book appointments for emergencies kind of defeats the purpose of having emergency services. Overall, it feels like it’s missing the mark on what’s really needed in acute care.
Terrifying. 3 years as an A+E Dr in the 90s before becoming a GP, and this algorithmising of people when they feel at their most vulnerable, disgusts me. Moronically thought up by an accountant, a manager, and a coder.
The new Govt better put a stop to this sort of shite.
Totally agree with Nick Mann.
I thought the issue is A/E exit not A/E entrance hence all the patients on trolleys.
Will those waiting for an inpatient admission bed be given the address of the local Dreams store and advised to go an lie down there instead?
It seems that many of these bonkers ideas stem from non-clinical managers/ICB leads/PCN leads blindly following following the advice of the “Fuller stocktake’. produced by NHS England in their ivory towers.
The patients will suffer at their unaccountable hands.
An absolute disgrace.
This is a blatant attempt to close the front door of A&E and transfer the workload to Primary Care. The LMC and GPC need to monitor this closely and ensure it doesnt become a template for wider rollout.
Things will go wrong, patients will be harmed and there will be near misses. They will go back to the old way then.
I have a new technique for doing a heart bypass operation – using toothpicks and coat hangers rather than sterile medical equipment
And a technique for preventing heart attacks which involves watching re-runs of Only Fools and Horses rather than cardiac rehab.
Both will save a lot of money, but nobody would let me do either without a range of high quality medical trials to prove they are effective, safe and cost effective.
I’ve also got a plan to reorganise the entire health system, which will save a lot of money. Luckily I don’t have to prove that is either safe, effective or indeed cost effective before I can get on with it.
What could possibly go wrong? except a doctor loses his license when this starts to fall apart and they are blamed for the problems caused by system failures to keep patients safe.
At first glance this appears to present a beautiful crafted plan to deal with the crisis of Acute Care. The whole premise of this argument is that people are attending EDs inappropriately Do we really still believe this? Of course there are all the usual suspects who should be somewhere else but they are a very small minority. Let’s call this out for what it really is Gatekeeping The real issue is capacity and this won’t solve it. The poor patients will be pushed from pillar to post trying to get help
*