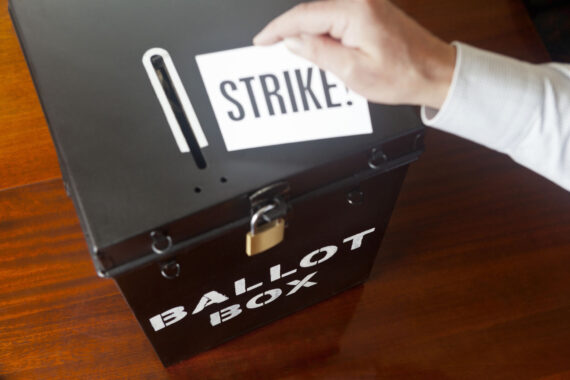
Exclusive Almost half (46%) of England’s GP practices are taking some form of collective action, with one in four putting a limit on the number of patients they see in a day, a Pulse survey has revealed.
The snapshot survey of 283 GP partners from different practices – representing 5% of the practices in England – found that two-thirds were either already limiting patient contacts, or were considering it.
Meanwhile, half (50%) of practices said they would be willing to escalate collective action, which could potentially involve full strike action, closing all services for a period of time.
The BMA’s GP Committee England launched collective action at the start of this month, with practices given the choice of which out of 10 potential forms of collective actions they would like to take.
Results of Pulse’s snapshot survey:
- 46% of the 283 practices in England who responded to our survey said they are currently taking some form of collective action
- A further 20% said they will be taking collective action in the future, and a further 22% said they were considering it
- Only 7% ruled out taking any action
- More than a quarter of all practices said they were limiting the number of patient contacts to 25 a day – a further 44% said they were considering whether to do so
- A quarter of GPs said they believe it will affect patient harm in the short term – but most feel it will improve, or won’t affect, patient harm in the short or medium term
- Half of GPs say they would be willing to escalate the level of collective action, including breaching contracts – which could involve closing their doors
A number of Pulse’s survey respondents said they were waiting for more guidance from local GP leaders before taking any collective action, or for practice colleagues to return from holidays.
All the actions outlined by the BMA are non-contractual, and a number of practices said they had already implemented them before the collective action was announced.
A GP partner in Staffordshire said: ‘I have been encouraged to take action by every single person who has asked.’
Another respondent, who wished to remain anonymous, said: ‘We have no wish to deny patients care whatsoever. It’s against our ethos.’
GPCE deputy chair Dr Julius Parker said: ‘We believe this very early survey demonstrates a strong commitment to collective action and that GPs are prepared to do whatever it takes to protect their patients and the future of general practice.’
He added that the GPCE has ‘always been clear that this action will be a slow burn, and its effect will be incremental’.
‘We also know and support the fact that colleagues will need time to consider how they want to take collective action.’
On the collective action options, Dr Parker said the intent is to ‘show NHS England and the Government what happens when GPs stop jumping through bureaucratic hoops and instead prioritise their patients’ needs, giving patients the time they deserve, instead of hurried consultations with tired doctors who are often working beyond safe working limits’.
He said: ‘GPs voted overwhelmingly in support for collective action and the profession is united in our goal: that general practice needs its share of the NHS pound to increase from 6p to 15p, while protecting existing funding across the wider system.
‘GPs are currently struggling to give patients the care they need. We can’t afford to hire staff, keep on top of rising running costs, or, in some cases, even stay open at all.’
Dr Amanda Doyle, NHS national director for primary care, said: ‘As some practices continue collective action, it is vital that patients continue to come forward for care in the usual ways – practices remain open and services are still running.
‘We will be monitoring the impacts of this action to ensure practices fulfil their contractual requirements and continue to meet the needs of patients.
‘The NHS remains committed to tackling the issues within general practice, and while changes have been introduced to help staff and improve patient access, we know general practice remains under significant pressure and is experiencing record demand, so we will continue to work together with GPs and other stakeholders to support the profession.’
Department of Health and Social Care spokesperson said: ‘This government is committed to shifting the focus of healthcare out of hospitals and into the community, to fix the front door to the NHS. We have already accepted the independent pay review body recommendation of a 6% uplift in GP pay and committed to hiring an extra 1,000 GPs into the NHS by cutting red tape, through an £82 million boost to the Additional Roles Reimbursement Scheme.
‘Collective action will only punish patients. NHS England has preparations in place to ensure patient safety is protected and patients should still come forward for care as usual.’
RCGP honorary secretary Dr Michael Mulholland said: ‘General practice is the front door of the NHS, but it has faced years of underfunding and neglect, and is now seriously struggling. We have raised significant concerns that the current GP contract is failing to provide GPs and their patients with the support that they need – and the decision to take collective action shows the strength of feeling amongst GPs across England.
‘It is not for the RCGP to get involved with contract negotiations between the BMA and NHS England, nor to influence how practices participate in collective action. No GP will want to restrict the services they provide for their patients, so we hope that the Government is able to intervene to help reach a fair resolution as soon as possible, so GPs have the funding and support to provide the care our patients need.’
Don’t miss: A longer data analysis of the survey findings will be published this afternoon.
The 10 collective action options recommended by BMA
- Limit daily patient contacts per clinician to a maximum of 25
- Stop engaging with the e-Referral Advice & Guidance pathway
- Serve notice on any voluntary services currently undertaken that plug local commissioning gaps
- Stop rationing referrals, investigations, and admissions
- Switch off GPConnect Update Record functionality that permits the entry of coding into the GP clinical record by third-party providers
- Withdraw permission for data sharing agreements that exclusively use data for secondary purposes (i.e. not direct care)
- Freeze sign-up to any new data sharing agreements or local system data sharing platforms
- Switch off Medicines Optimisation Software embedded by the local ICB for the purposes of system financial savings and/or rationing
- Defer signing declarations of completion for “better digital telephony” and “simpler online requests” until further GPC England guidance is available
- Defer making any decisions to accept local or national NHSE Pilot programmes whilst we explore opportunities with the new Government
This survey was open between 8 and 12 August 2024, collating responses using the SurveyMonkey tool. After removing duplicate entries from the same practice, a total of 283 GP partners from England responded to these questions. The survey was advertised to our readers via our website and email newsletter, with a prize draw for a £150 John Lewis voucher as an incentive to complete the survey. The survey was unweighted, and we do not claim this to be scientific – only a snapshot of the GP population.
Note: This story was updated at 12.41 on 13 August to reflect that one in four are capping patient contacts. A previous version of the story’s introduction had said one in five.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens