Welsh health boards have been told to develop plans within three months to help GPs make the most use of advice and guidance (A&G), to improve NHS productivity and reduce hospital referrals.
Health secretary Jeremy Miles has accepted 29 recommendations made by the ministerial advisory group (MAG) on NHS performance and productivity, which was set up in October to ‘look at the effectiveness of current NHS Wales arrangements’.
The review, led by former chief operating officer of NHS England Sir David Sloman, focused on planned care, diagnostics, cancer performance and urgent and emergency care and considered ways to ‘improve productivity and performance’.
It found that in some health boards up to 40% of contacts between GPs and consultants are via e-advice, while in other health boards electronic triage or grading of referral letters is ‘not taking place’, with a ‘continued heavy reliance on traditional paper-based systems’.
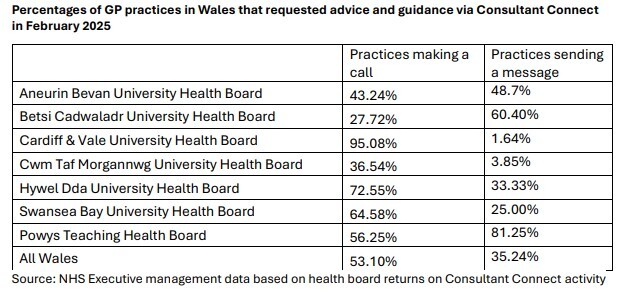
It pointed to A&G data for each health board (see table), which showed that across Wales 53% of practices requested it via ‘making a call’, while 35% via ‘sending a message’.
‘The MAG can see no reason why all health boards should not meet the level of the highest user,’ it added.
It recommended that all health boards should ‘within three months’ develop a plan to reduce referrals to traditional outpatients in ‘high volume specialities’ and that models to offer alternatives to referrals should be ‘identified and scaled’.
The Welsh Government should also continue to provide national funding for A&G, it added.
The report said: ‘The MAG believes that there is significant potential for reducing referrals to secondary care if all health boards adopt the range of interventions available.
‘This includes full adoption of the national community health pathway programme and full deployment of advice and guidance. The national funding for these schemes needs to continue.’
In response to this recommendation, which was accepted in full, the Welsh Government said health boards are ‘expected to identify and tackle unwarranted variation’ in referral rates from GP practices and that progress ‘will be monitored’.
It said: ‘Delivering on this recommendation is an implementation requirement for health boards who should set out clear delivery plans to the proposed timescales which should be progressed through their response to the priority enabling actions.
‘High referral rates may well be warranted within population groups, and the report sets out that it is the unwarranted variation that must be addressed.
‘Therefore, health boards are expected to identify and tackle unwarranted variation in implementing this recommendation. Progress will be monitored and reviewed through health board performance meetings.’
It comes after the Welsh Government said earlier this year that it will not increase the share of NHS funding spent on general practice until hospital waiting lists are ‘brought down’.
Health secretary Jeremy Miles said: ‘The message in the report is very clear: we have a significant challenge in performance and in productivity. The service is not performing at the levels that we or the public need and expect it to.
‘That demands a step change in our approach so we can improve the services the public receives, deliver better health outcomes they deserve, and make sure every pound spent brings the best value, as demands on the health service increase into the future.
‘But the report is also optimistic. Time and again it outlines the strength of the assets we have in Wales. It highlights the commitment and skill of our staff – clinical and managerial – of good strategy, and often of good practice.’
The recommendation in full
All health boards should, within three months, develop a plan to reduce referrals to traditional outpatients in high volume specialities. Particular attention should be given to unwarranted variation and specialities where per capita referrals rates are above the national median.
Models that offer alternatives to traditional outpatient pathways should be rapidly identified and scaled. National Funding for Advice and Guidance and the National Pathways programme should continue.
From June 2025, progress should be reported monthly to health board and trust public meetings, and at individual monthly Performance & Productivity meetings.
Source: Ministerial Advisory Group report














