This site is intended for health professionals only
Frailty hubs are the focus of integrated neighbourhood teams (INT) in Surrey where the author of the Fuller Stocktake, which first mentioned the idea, heads up the NHS.
Delegates at Pulse PCN London heard from East Surrey’s Care Collaborative PCN clinical director Dr Pramit Patel about the area’s INTs.
The idea was first suggested in the Next steps for integrating primary care: Fuller Stocktake report, written by Professor Claire Fuller, CEO of the Surrey Heartlands integrated care board (ICB).
Dr Patel explained that from a population of 200,000 in East Surrey, 62,400 were identified as high users of healthcare services and of those patients 1% or 624 had 1,900 A&E attendances, 500 ED attendances 500 outpatient appointments and admissions, and 54,000 primary care contacts in the past 12 months.
‘Further analysis found that 75% of that cohort were frail so we thought about how to start reducing all that activity and actually get the care that person really needs,’ said Dr Patel, who is also the primary care representative on the ICB.
Building on work done with The King’s Fund, using the Primary Care Home model, East Surrey has now set up an anticipatory care hub in each PCN. These hubs are built around a lead GP, care coordinators, physician associates and pharmacists from the additional roles reimbursement scheme (ARRS), along with a geriatrician, hospice representatives and community matrons working with a multidisciplinary team, including social care and dental surgeons.
This was initially funded by £300,000 of seed money from transformation funding secured in 2019 from the integrated care system (ICS), then still a clinical commissioning group. This paid for a GP in each of East Surrey’s five PCNs for three days a week (£60,000).
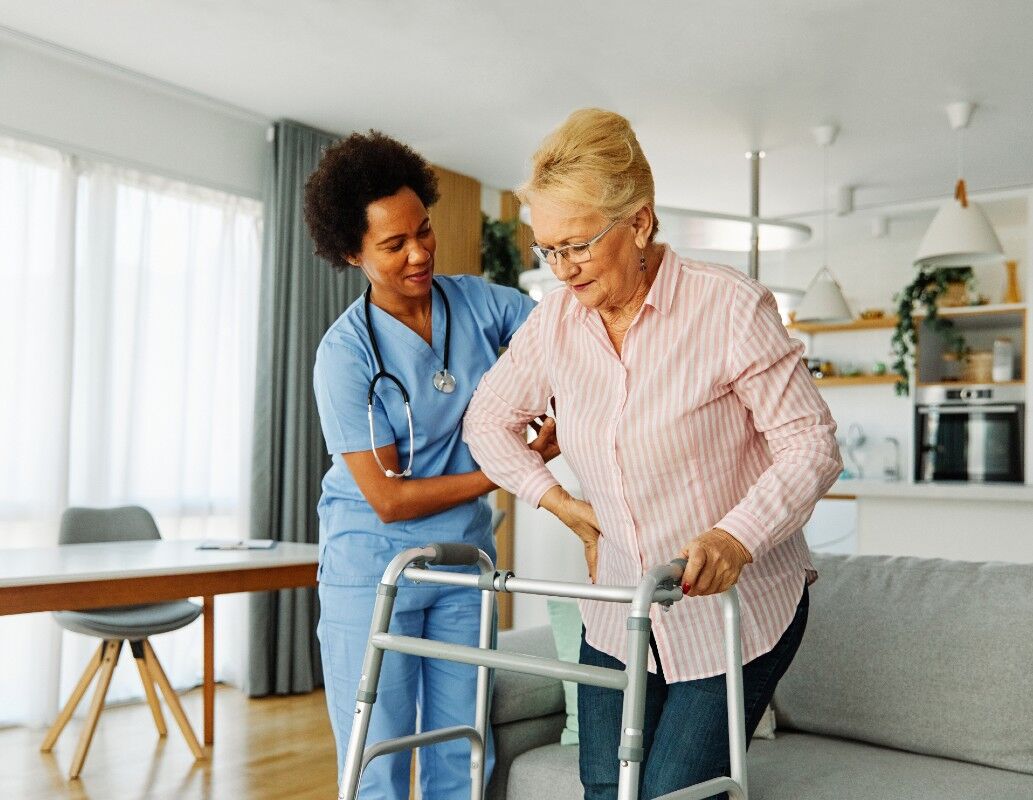
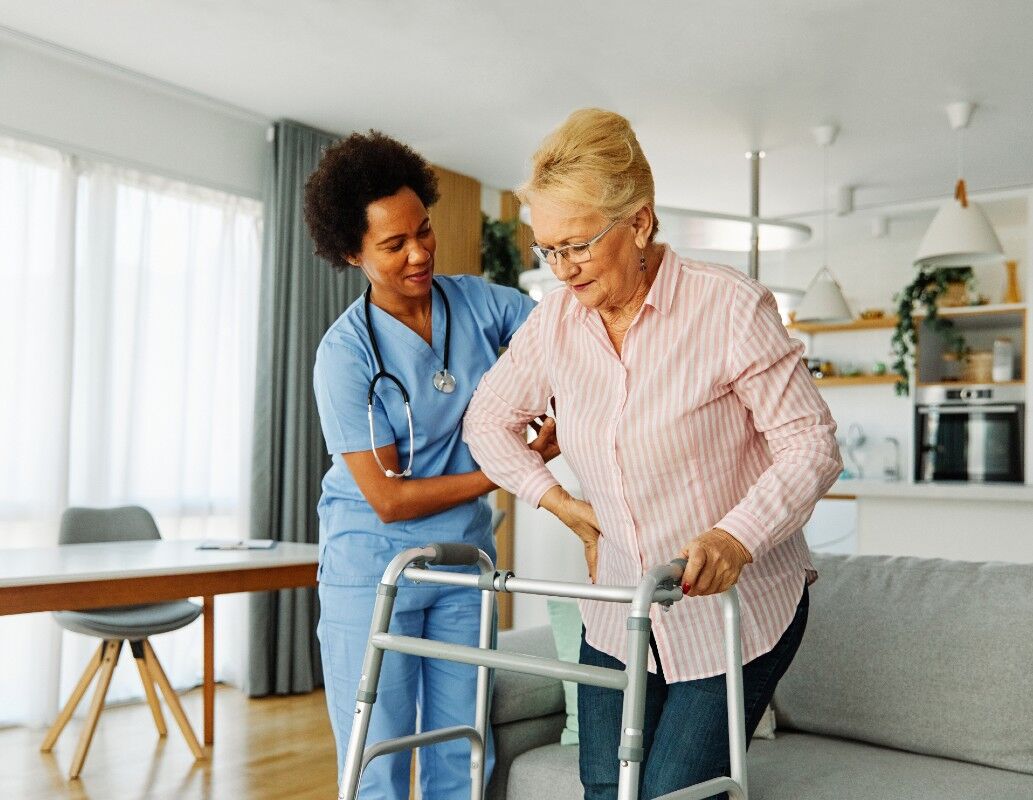
‘If you’re an elderly patient and you’re moderate to severe frail, you will be identified and a physician associate or community matron will go out and do a comprehensive geriatric assessment. They’ll go out into the patient’s home and spend a good hour and a half there and they will then do that proactive, anticipatory care work, and bring in the right agency.
‘So if you’ve identified that they’re isolated, we bring in a befriending service or a wellbeing service. If they’ve got care issues we’ve now got links to social care, so we can talk to that representative in the hub,’ said Dr Patel, adding that, rather than the duty doctor getting called out and spending five minutes with a patient, now the call comes to a care coordinator who works out who is best to go out, as they know the patient and their circumstances.
‘If it is felt they need an admission the urgent care response team will go out within two hours and hopefully keep that patient at home, so they will onboard them to the virtual ward or admit them to the acute,’ he explained.
Through this way of working there has been a ‘massive’ drop in A&E attendances of 17% and a drop in admissions of 13% in this cohort of patients. Dr Patel said that data like this can be used as evidence to the ICB of a return on investment and make the case for continued or increased funding into primary care.
Pulse PCN London delegates also heard about the future of PCNs from consultant Ben Gowland who said that with integration top of the agenda, the ‘system does not want to revert to dealing with 6,500 practices instead of 1,250 PCNs. He believes that it is ‘highly unlikely PCNs are going anywhere in the short term, and the group working model is likely to be strengthened, with more focus on joint working with local community teams and INTs most likely to develop locally, rather than be imposed’.
Pulse PCN events are forums which take place across England and are designed to support and inform clinical directors and those working at scale in primary care. To find out more click here.