How we established our consultant-led surgery

James Foster, executive manager of St Stephens Gate Medical Practice in Norwich, shares how day surgery in the community can save money, increase capacity and give GPs resilience
Like many GP practices, we take what we do for granted. It was only when a BBC reporter rang us that we realised we had a story to tell. We had repaired her producer’s hernia, he had casually mentioned the experience to her, and she was on the phone to us pronto.
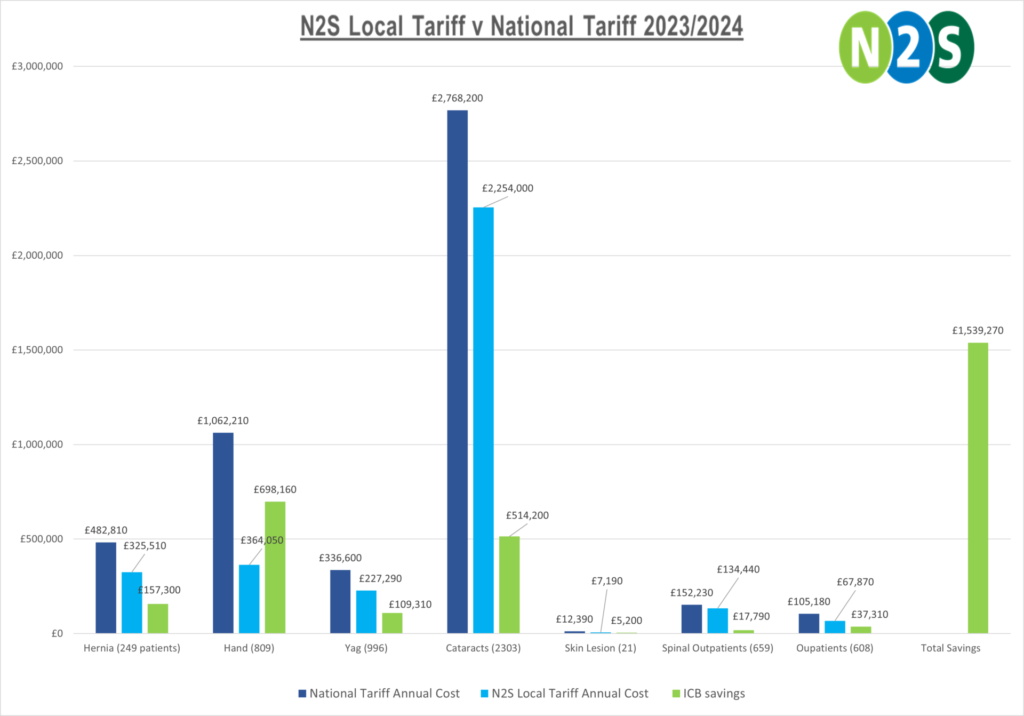
Our surgery, under the banner of N2S, performs thousands of consultant-led surgical procedures every year, saving our ICB £1.5 million a year. We started a little over 10 years ago, as a box file in an office corner. How did it grow, and can anyone do it?
At a first glance, St Stephens Gate Medical Partnership isn’t different from any other mid-sized urban practice. We are a GMS practice serving around 19,000 patients with a mixed population in a modern purpose-built health centre.

What is different is that we provide around 7,000 consultant-led NHS day surgery procedures a year under the brand name of N2S. The service started in 2011 as one cataract list a fortnight, but has grown to nine or 10 theatre days a week covering eyes, hands, skin, hernias – and recently work with the East of England spinal team. Several of these surgical procedures have been switched off at the local hospitals. We exist as a normal referral destination on the national electronic referral service.
Our driving force has been to be considered a full member of the local NHS family. The service is overseen by GPs and expert managers. We have always prioritised patient experience, responsiveness and being good value for money.
The world of surgical funding is complex, and usually payments are made at a higher national tariff rate. N2S has always offered commissioners lower Blended or Local Tariff prices, which means for some services we are doing procedures for less than half the price of other independent sector providers (ISPs) or the hospital. That is why we have been able to deliver commissioners around £1.5 million in savings per year for the work we undertake.
N2S is run alongside our primary care activity by the GP partnership. We have some admin staff who are dedicated to the surgical side but many move between the two. The blend of services adds vibrancy to the working day. St Stephens Gate is a learning organisation offering teaching and training; this is replicated at N2S with surgical training opportunities, participation in academic research with contributions to the British Association for Day Surgery and being showcased at National Conferences.
One of the criticisms of the community model is that they don’t provide training, but we offer training on every single clinical activity that happens on the site.
We believe that primary care and hospitals working together is the best possible solution to funding cuts across the board. For us, we have created capacity, cut waiting lists, and saved money. At the same time, it has made our own practice more stable, vibrant, and resilient.
One of our best achievements is expanding capacity during Covid to support local hospitals. We have continued this by supporting waiting list recovery and have provided additional Yag Laser, Cataracts and spinal appointments to patients who had waited for up to 72 weeks.
N2S was fully operational within 10 weeks in response to Covid. As soon as lockdown hit, we adapted and re-designed our pathways. We found that we could deliver the same level of activity without compromising on safety and have kept most of our Covid adaptations in place as they made our pathways much more efficient.
One service that we are proud of is that we have taken more than 600 spinal patients from the hospital waiting list, and we are now talking to the ICB to offer an image-guided injection pathway at N2S to create a much-needed treatment to patients with back pain. We are also in active discussion with our urology and gynaecology colleagues.
This is an example of why general practice often shows excellent levels of resilience and flexibility – and why GPs deserve to be given a bit of help to become involved with community services.
We are very grateful that the Norfolk and Waveney ICB (and the CCG before them) have been so forward thinking in their ongoing support. We also have an excellent working relationship with our landlords who supported the creation of three extra consulting rooms, increased our admin space, as well as building a second theatre.
Many GP new builds have an unused theatre, so there is capacity. We think that what we do could be replicated across the UK with the support of NHS England and ICBs and create similar excellent value for money services in GP settings.
As often quoted by NHS Confed: Every £1 invested in the community yields £14 in return. One hundred practices doing what we do is 700,000 more surgical patients seen and treated every year. General practice has shown time and again that with a little support we can deliver a lot. Our journey hasn’t been easy and has taken a lot of hard work. But then again, general practice has never been a walk in the park.
Pulse October survey
Take our July 2025 survey to potentially win £1.000 worth of tokens

Related Articles
READERS' COMMENTS [1]
Please note, only GPs are permitted to add comments to articles











What would be the effect on the hospital system which would have lost funding?
I don’t know of a local GPs surgery that has an unused ‘Theatre’ with all resources available – although our cotage hospitals used to have them, which was very useful to save patients trips to distant hospitals, and expecially useful out of hours.